
Healthcare Payer Data Analytics and Data Management
Healthcare payer data analytics management is crucial in optimizing payer operations and improving patient outcomes. By harnessing the power of data, payers can gain valuable insights into patient populations, identify high-risk patients, and make informed decisions that lower costs and improve care.
The data analytics space is fraught with challenges, however. Fragmented data sources, limited data interoperability, and a lack of talent to perform advanced analytics capabilities make it challenging for payers to accomplish their goals.
To overcome these issues, payers need to invest in robust data integration and analytics solutions that leverage data to drive better health outcomes and financial performance. We will take a look at the systems and strategies that will help payers get a grip on their healthcare data analytics programs.
The Benefits and Challenges of Data Analytics |
|
|
Healthcare Analytics Use Cases/Beneficial Outcomes |
Challenges |
|
|
How To Delegate Resources For Healthcare Payer Data Analytics
Efficient resource delegation is key to helping payers keep operational costs in check. Data analytics and customer experience teams often take up a healthy portion of an organization's resource budget due to the high cost of expertise in this space. Payers need to rely on sound data management strategies and look for areas of automation to mitigate inflated costs. As organizations face increased government regulation on healthcare data compliance and internal pressure to cut operational costs, payers can focus on maturing their systems to meet these demands. Payers need to focus on mature systems that encourage the evolution of digital healthcare trends and regulations. Even when payers are able to achieve this and assign data analytic resources properly, it still ends up being a relatively large project to maintain over time.
Payers work with large datasets that include personal identifiable information (PII) on each member. These datasets need to be maintained and secure while users access, integrate, cleanse, govern, store, and prep data.
To improve data integrity, payers need to find the right data analytics tools and strategies to do the job.
The main data that payers collect is:
- Clinical data
- Financial data
- Socioeconomic data
Different data will need to utilize different tools and systems. Experimenting with different digital strategies can help payers optimize procedures, ensuring each process of the data lifecycle is enhanced for the most thorough analysis.
Data Analytic Strategies to Manage Risk
CIOs look to improve healthcare payer data analytics by implementing systems, strategies, and frameworks that mitigate risk and benefit customer satisfaction. Data analytic strategies look to improve data content, quality, ownership, governance, security, and provisioning. These are some that can be used to help relieve some of the doubts and challenges of big data analytics.
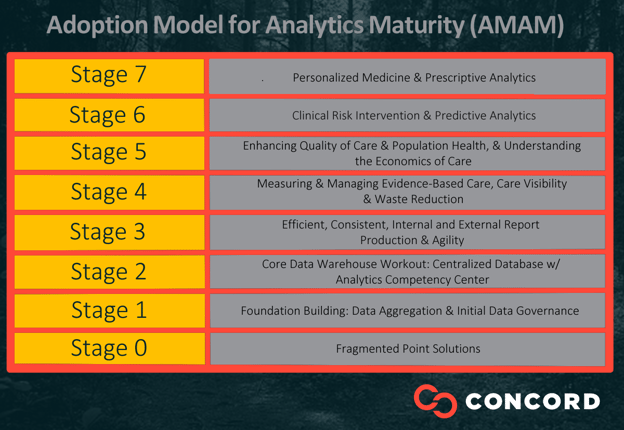
- Implementing the Adoption Model for Analytics Maturity (AMAM) by HIMSS is considered a best practice because it helps payers improve predictive analytics and governance and workforce dimensions. AMAM is a framework, categorized by stages, for how healthcare organizations can measure their analytics capabilities regardless of the technology incorporated in the organization's architecture.
- Build a data governance strategy to govern data quality, integrity, access, and security. This should become a central component of your organization's workflow.
- Assign data classifications to each data instance. This will allow you to be more precise with data predictions and organization by increasing the context, quality, and usability of each instance.
- Leverage machine learning in data management to help your teams streamline the analysis process. Machine learning tools can also improve prediction analytics by harvesting larger quantities of both unstructured and structured data.
Optimize Healthcare Payer Data Analytics and Services With Concord
Healthcare payer data analytic strategies can improve administrative efficiency and customer satisfaction. By nurturing data integrity, payers can make better decisions on members' claims and applications.
Whether you are looking to maintain a mature data architecture or experiment to optimize and delegate resources for healthcare payer data analytics, Concord can guide you every step of the way.
Getting Started
Concord USA is a consultancy that combines technology and industry depth with a get-it-done culture to enable resiliency, efficiency, and innovation. Whether you are trying to improve customer satisfaction, data strategies, security, or other technological issues, Concord can help.
Contact us today to learn more about the benefits of healthcare payer data analytics, our Technology Integration Services, and how we can help your business thrive.