
How to Use Value-Based Care Data Analytics to Improve Customer Satisfaction
Data analytics directly affect the success of payers in delivering care that meets member needs and expectations. One way payers prioritize their efforts to improve member satisfaction is by moving away from fee-for-service care models towards value-based care models. One of the most effective ways to make this transition successful without reducing member satisfaction is through the use of value-based care data analytics.
The Role of Value-Based Care Data Analytics in Customer Satisfaction
By leveraging data analytics, healthcare payers can gain invaluable insights into member behavior, preferences, and experiences. These insights can help payers identify areas of improvement to drive better care outcomes and increased star ratings. However, while many healthcare payers are aware of the importance of data analytics, they may not know where to begin with leveraging insights.
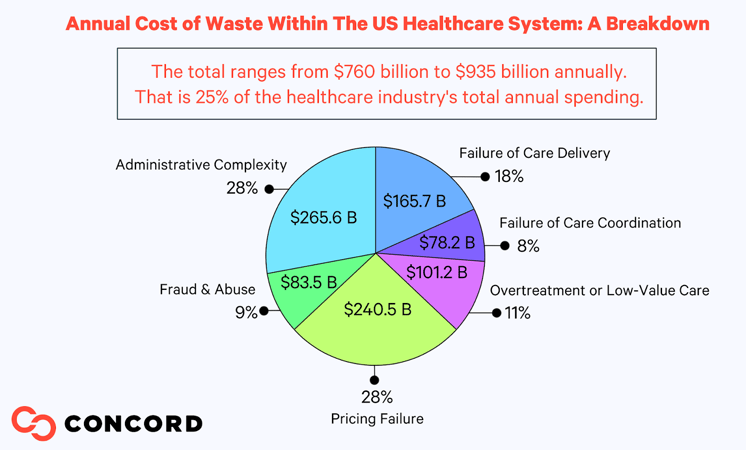
Members don’t want to continue paying for services that do not benefit their health. Luckily, value-based care data analytics can save payers from wasting opportunities for care delivery and coordination. The estimated cost of waste in the US healthcare system ranges from $760-$935 billion annually. That is 25% of the healthcare industry's total annual spending. By following consistent data gathering and application analytics methods, payers can pinpoint patterns of waste to help prevent further loss over time and determine gaps within their member's care.
Analyze and Utilize Data For The Transition To Value-Based Care
While value-based care is estimated to help payers in the long run, payers may see revenue shortfalls in the short run. Data analytics can provide payers with insights on how to assess care during the revenue transition period while they are moving from fee-for-service to value-based care profitability.
What To Assess
It’s important not to add to cost waste by assessing the wrong data. Instead, payers should focus on understanding the context and purpose of the data to ensure its relevance. They must identify the source of the data, its quality, and any potential biases that could affect the results.
The Centers for Medicare and Medicaid Services (CMS) identifies the quality measures of care that payers should assess through value-based care data analytics to help cultivate the results in customer satisfaction they are looking for. These are:
- Effectiveness of care
- Timeliness of care
- Efficiency of care
- Safety procedures
- Equitability
How To Interpret
When interpreting data, payers should adopt a systematic and analytical approach to extract valuable insights and make informed decisions. By employing appropriate statistical methods and tools to analyze the data effectively, payers are able to view:
- Patterns
- Trends
- Correlations
This will help payers identify key factors impacting healthcare costs, utilization, and outcomes.
Payers should also consider benchmarking the data against industry standards and best practices to gain a broader perspective in accordance with value-based care. By collaborating with data scientists, analysts, and specialty consultants, payers can gain deeper insights and validate their findings.
Where To Implement
Payers should translate the data into actionable strategies and interventions. By interpreting data thoughtfully, payers can enhance their decision-making processes, improve healthcare outcomes, and optimize resource allocation to benefit patients, providers, and the entire healthcare ecosystem.
By implementing the interpretations of value-based care data analytics, such as the CMS quality measures and member needs, payers can identify and provide coverage for care facilities that are up to standard to benefit their star ratings, member satisfaction, and preventative cost measures.
Value-Based Care Data Analytics: Best Practices
Several best practices should be followed for value-based care data analytics to ensure successful implementation. These include:
- Establish clear goals and objectives for data analytics to precisely align with the principles of value-based care. This includes defining specific metrics and outcome measures that align with quality improvement, cost reduction, and patient satisfaction.
- Refine data models frequently. This includes updating risk stratification algorithms, predictive models, and performance metrics to reflect changing patient populations, clinical guidelines, and care pathways. By regularly monitoring and evaluating data analytics, payers can identify areas for refinement and continuous improvement to ensure they capture the most relevant and up-to-date information to drive decision-making.
- Prioritize data integration from various sources, such as electronic health records, claims data, and patient-generated data, to obtain a comprehensive and holistic view of patient care. Utilizing advanced analytics techniques, such as predictive modeling and machine learning, can provide valuable insights for risk stratification, care management, and population health interventions.
- Implement data governance policies and procedures to ensure data accuracy, privacy, and compliance with regulatory requirements.
- Invest in robust data infrastructure and technology systems, such as those listed below that can securely collect, store, and process large volumes of data. Technical tools, such as automation processing tools, data consolidation tools, and easy-to-use APIs, can also be added to your existing systems to encourage interoperability.
- Speak to specialty tech consultants to ensure the data management strategy is optimized and works towards the future of value-based care. They can assist in identifying the right data analytics solutions and tools tailored to their specific needs, ensuring efficient data collection, storage, and analysis.
Value-Based Care Data Analytics: Tools and Added Solutions |
||
|
Salesforce |
Salesforce is a cloud-based software that is the global leader in Customer Relationship Management (CRM) software and applications. Utilize Salesforce to gain a complete understanding through data analytics of your member's needs, pain points, and more. |
|
|
Snowflake |
Snowflake is a cloud computing based data company that provides the only data warehouse built for any cloud. Snowflakes Cloud Data Platform helps payers derive all the insights about their members into one platform safely in the cloud. |
|
|
Tealium |
Tealium is a customer data platform (CDP) that works with your data so you can connect with your members. Tealium’s Customer Data Platform, Tag Management, and Event Streaming solutions help payers build out a 360-degree view of their customers to help identify weak points in their provided care. |
|
By following these best practices, payers can effectively leverage data analytics to enhance their transition to value-based care, improve patient outcomes, and optimize healthcare resources.
Get The Most Out of Your Data Analytics For Value-Based Care
Consultants can guide payers in establishing a roadmap for transitioning to value-based care, all through value-based care data analytics. Get the most out of your data analytics for value-based care when you partner with Concord.
Concord USA is a consultancy that combines technology and industry depth with a get-it-done culture to enable resiliency, efficiency, and innovation. Whether you are trying to improve customer satisfaction, data strategies, security, or other technological issues, Concord can help.
Contact us today to learn more about value-based care data analytics, our technology integration services, and how we can help your business thrive.